Eating should feel simple, but acid reflux can turn meals into a daily challenge. I used to think skipping foods was the only answer, until structure made things easier.
A 7-day acid reflux meal plan helps remove guesswork by setting steady meals, calmer food choices, and better timing, especially when you understand basics like the best bread for GERD and how simple grains affect digestion.
You may notice symptoms show up after late dinners, heavy portions, or certain ingredients, which makes eating feel stressful. That is where a clear plan can help bring some control back.
This approach focuses on gentle meals, repeatable routines, and flexibility when something does not sit well. With the right setup, meals can feel more manageable again, and this 7-day acid reflux meal plan shows how to start.
Who is the Best Fit for This 7-Day Acid Reflux Meal Plan
This meal plan suits people dealing with mild to moderate acid reflux who want a clear structure without strict limits. It works well if symptoms tend to flare after large meals, late dinners, or high-fat foods.
The plan fits home cooking routines and relies on common ingredients that are easy to prepare.
It may help if heartburn shows up several times a week, but is not constant throughout the day. This approach also suits anyone wanting to test food tolerance in a short, controlled way.
Adjustments may be needed for severe symptoms, pregnancy, recent digestive surgery, or other medical conditions.
A healthcare professional should always check ongoing discomfort, trouble swallowing, or chest pain before relying on dietary changes alone.
Your 7 Day Acid Reflux Meal Plan
This section shares a complete seven-day meal plan with clear structure, gentle foods, and flexible options to support daily symptom control.
How to Use This Plan
Follow this plan with three steady meals and one or two snacks each day to avoid large gaps or heavy portions. Portions can be adjusted based on hunger, energy needs, and comfort after eating.
Try to finish the last meal at least three hours before lying down to reduce nighttime symptoms. If any food causes discomfort, use a similar swap instead of forcing it.
Meals are meant to feel repeatable, simple, and realistic for daily routines. Cooking methods should stay basic, such as baking, grilling, or steaming, to keep meals easier to digest throughout the week.
Day 1

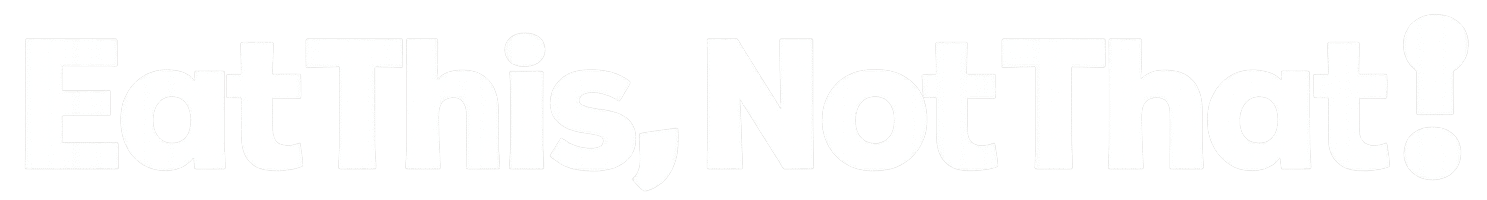
Breakfast can include oatmeal with banana or a spinach egg dish with melon. Lunch may be a chicken and vegetable soup or bean toast with yogurt.
Dinner works best with baked fish, quinoa, and cooked vegetables. Snacks can include a pear, almonds, or yogurt.
Dessert should stay light, such as yogurt with honey. Focus on slower eating and moderate portions. This first day helps settle digestion and sets the rhythm for the rest of the week without heavy seasoning or late meals.
Day 2

Start with oatmeal topped with berries or yogurt with melon. Lunch may repeat a broth-based soup with bread or a turkey wrap with mild fillings. Dinner can include baked chicken with rice and green beans.
Snacks may include apple slices, edamame, or yogurt. Dessert should remain simple and low-fat. Keep fluids spaced between meals rather than during meals. This day builds consistency and keeps meals predictable, which often helps reduce mid-day discomfort.
Day 3

Breakfast works well as a low-acid smoothie or eggs with toast. Lunch may include soup with whole-grain bread or a grain bowl with vegetables.
Dinner can feature pasta with a mild cheese sauce or shrimp with quinoa, and choosing simple shapes and lighter sauces can help if you are unsure whether pasta for acid reflux feels comfortable.
Snacks may include crackers with cheese or fruit. Dessert can be baked fruit with cinnamon. This day supports balance by mixing plant-based meals with simple protein options while keeping fat and spice levels steady.
Day 4

Begin with yogurt and berries or a spinach egg meal. Lunch may include tuna over greens or leftover soup with fruit. Dinner can feature turkey patties with potatoes or a bean-based taco using mild toppings.
Snacks may include cottage cheese or a pear. Dessert should stay gentle and low acid. Pay attention to meal timing on this day, especially in the evening, to help reduce overnight discomfort and support better sleep.
Day 5

Breakfast may repeat oatmeal with fruit or yogurt mixed in. Lunch can include a chicken and grain salad or soup with bread. Dinner may feature baked white fish with sweet potatoes and cooked vegetables.
Snacks may include cucumber slices or yogurt. Dessert can be fruit or yogurt. This day continues variety while keeping foods familiar. Repeating meals that feel comfortable can help reinforce patterns that reduce symptoms during the week.
Day 6

Start with yogurt and nuts or toast with egg. Lunch may include a vegetable wrap or soup with a simple salad. Dinner can feature pork or tofu with potatoes and vegetables. Snacks may include fruit with nuts or hummus with vegetables.
Dessert should remain light and low-fat. Focus on staying upright after meals and avoiding large portions late in the day, as symptoms may be more noticeable by this point.
Day 7
Breakfast may include eggs with melon or a chia-style pudding with fruit. Lunch can be a grain bowl with beans or a wrap with mild fillings. Dinner works best with baked fish, rice, and cooked vegetables.
Snacks may include edamame or fruit with crackers. Dessert should stay gentle and simple. This final day helps confirm which foods feel most comfortable and which may need limits moving forward.
Use this seven-day table as a simple reference for daily meals. Portions can be adjusted, and swaps may be used if symptoms appear.
| Day | Breakfast | Lunch | Dinner | Snacks | Dessert |
|---|---|---|---|---|---|
| Day 1 | Oatmeal with banana | Chicken soup with bread | Baked fish with quinoa and vegetables | Pear, almonds | Yogurt with honey |
| Day 2 | Yogurt with melon | Turkey wrap with cucumber | Baked chicken with rice and green beans | Apple slices | Baked fruit |
| Day 3 | Eggs with toast | Soup with whole-grain bread | Pasta with mild cheese sauce and greens | Crackers, fruit | Cinnamon apple |
| Day 4 | Yogurt with berries | Tuna over greens | Turkey patties with potatoes | Cottage cheese | Yogurt |
| Day 5 | Oatmeal with berries | Chicken grain salad | White fish with sweet potatoes | Cucumber slices | Fruit |
| Day 6 | Toast with egg | Veggie wrap | Pork or tofu with vegetables | Nuts, fruit | Yogurt |
| Day 7 | Eggs with melon | Bean and grain bowl | Baked fish with rice and vegetables | Edamame | Light yogurt |
Repeat meals that feel comfortable, note foods causing discomfort, and use this plan as a base for future weeks if symptoms improve.
How This 7 Day Plan Helps Reduce Acid Reflux
This section explains why certain food choices and eating habits are used, and how they may support better digestion and fewer reflux flare-ups over time.
Food Patterns This Plan Focuses On
This plan centers on foods that tend to sit more comfortably in the stomach and reduce excess pressure. Higher fiber foods help manage hunger, which lowers the chance of overeating.
Lean protein options keep meals filling without adding heavy fat. Low-acid and mild foods are used to reduce irritation in the throat and chest.
Meals are balanced with simple grains, cooked vegetables, and gentle fruits, which can support steadier digestion and reduce sudden symptom spikes during the day.
Eating Habits Built Into the Plan
Beyond food choices, daily habits play a major role in symptom control. Meals are spaced evenly to avoid long gaps followed by overeating. Portions stay moderate to reduce stomach pressure after eating.
Late-night meals are avoided to limit nighttime symptoms. Cooking methods stay simple, using baking, grilling, or steaming instead of frying. Mild herbs replace heavy sauces or spices, helping meals stay easier to tolerate while still feeling satisfying and complete.
How Fast You May Notice Changes

Changes from a structured acid reflux meal plan often happen gradually rather than all at once.
During the first one to two days, some people notice less fullness, pressure, or discomfort after meals, especially when portions stay moderate.
By days three to four, symptoms between meals may feel less intense, and nighttime discomfort may ease if late eating is avoided.
Toward the end of the week, patterns often become clearer, making it easier to spot foods or habits that trigger symptoms. Results vary based on digestion, stress levels, meal timing, and food tolerance.
Some days may feel better than others, which is normal. Keeping meals consistent and tracking symptoms can help make sense of these changes. If symptoms remain strong, worsen, or interfere with daily life, medical advice is important.
Trigger Food Swaps (Use This If Something Bothers You)
Some foods cause symptoms even when meals look balanced. Swaps help keep meals comfortable without skipping food. Changes work best when done one item at a time
Common food swaps to try
- Tomato-based sauces → Olive oil with herbs or mild yogurt sauce
- Citrus fruit → Banana, melon, or pear
- Fried foods → Baked, grilled, or steamed options
- Spicy seasoning → Mild herbs like parsley, dill, or basil
- Chocolate desserts → Yogurt with honey or baked fruit
- High-fat meats → Chicken breast, fish, beans, or tofu
- Test swaps earlier in the day when symptoms are easier to track
- Keep portions moderate when trying something new
- Note reactions over the next 24 hours before making another change
What to Eat on a Bad Reflux Day
Some days, symptoms feel stronger even when meals are usually well tolerated. A bad reflux day calls for a simpler approach that gives the digestive system a break.
The goal is to lower irritation, avoid pressure in the stomach, and keep meals easy to handle. Choose soft, low-fat foods and spread intake across small portions rather than full plates.
Warm, plain meals often feel better than cold or heavy foods. Focus on calm eating, slow pacing, and upright posture after meals.
A gentle day may include oatmeal or plain toast for breakfast, followed by broth-based soup, rice, or potatoes later on. Bananas, melon, or cooked apples can work as fruit options.
Yogurt may feel soothing for some people. Skip coffee, rich sauces, fried foods, and strong seasonings, even if they are sometimes tolerated. Once symptoms settle, regular meals can slowly return.
Eating Habits That Matter as Much as Food
Daily eating habits affect reflux symptoms just as strongly as food choices, especially meal timing, posture, portion size, and pacing.
Before Meals
What happens before eating can shape how the body handles food. Large snacks close to meals can increase stomach pressure once eating begins. Leaving space between snacks and meals helps digestion start smoothly.
Staying upright before meals also matters, since slouching or lying down can slow stomach emptying. A calm start sets better conditions for digestion and reduces early discomfort once eating begins.
During Meals
Eating speed and portion size strongly influence symptoms. Eating slowly allows the stomach to process food without sudden overload. Overeating stretches the stomach, which can push contents upward and trigger discomfort.
Limiting drinks during meals helps prevent excess volume from building too quickly. Smaller sips taken between meals often feel easier than large glasses during eating.
After Meals
Post-meal behavior plays a major role in symptom control. Remaining upright for at least 30 to 60 minutes allows gravity to support digestion. Lying down or bending soon after eating can force stomach contents upward.
Light walking or sitting upright can help food move forward naturally and reduce pressure in the chest or throat during digestion.
Before Bed
Evening habits often affect nighttime symptoms. Finishing food intake three to four hours before bed allows the stomach time to empty. This reduces the chance of discomfort while lying down.
Raising the head of the bed can help keep stomach contents from moving upward during sleep. Late snacks and heavy meals are best avoided when symptoms tend to appear overnight.
Meal Prep Tips to Make the Week Easier
Planning ahead reduces daily cooking stress and helps keep meals consistent, simple, and easier to manage during busy or low-energy days.
- Prepare one large pot of soup to cover several lunches or dinners during the week.
- Cook grains like rice or quinoa in advance and store portions in the fridge.
- Roast mixed vegetables on one tray to use across multiple meals.
- Wash, cut, and store fruits early for quick snacks.
- Portion nuts, yogurt, and hummus ahead to avoid overeating.
- Keep backup meals ready for days when cooking feels difficult.
GERD Friendly Eating When You are Not Cooking
Eating away from home can feel challenging when acid reflux is a concern, but simple choices can still help manage symptoms. Focus on meals that are baked, grilled, or steamed rather than fried.
Plain proteins, cooked vegetables, rice, and potatoes often work better than heavily seasoned or rich dishes. Ask for sauces and dressings on the side so portions stay controlled.
Avoid large meals and consider sharing or saving part for later. Eating slowly and staying upright after meals remains important even when dining out.
For quick service options, oatmeal, plain sandwiches, grilled items, or soup can be easier to tolerate. Skipping late-night meals and choosing water or mild tea instead of carbonated drinks may also reduce discomfort.
Planning ahead and keeping portions moderate can make eating out feel more manageable.
GERD and IBS: What to Know
GERD and IBS are different digestive conditions, but symptoms can overlap in some people. GERD mainly affects the upper digestive tract and often causes burning in the chest or throat.
IBS usually affects the lower digestive tract and may involve bloating, gas, constipation, or loose stools. Because symptoms can occur together, food choices that help one condition may not always help the other.
For example, smaller meals and steady timing may support both, while certain high fiber foods may ease reflux but worsen bowel symptoms for some people.
Care is needed to avoid cutting out too many foods at once, which can lead to limited nutrition and added stress. Keeping meals simple, tracking symptoms, and changing one food at a time can help identify what works best.
A healthcare provider should review ongoing or severe symptoms for proper guidance.
Conclusion
Managing reflux often comes down to steady habits rather than perfect meals. This guide covered simple food choices, daily structure, meal timing, swaps, and backup options for harder days.
The goal is to make eating feel predictable and less stressful, while helping spot what supports better comfort.
A 7-day acid reflux meal plan can act as a short reset, giving space to notice patterns without cutting out everything at once. I find that small changes, repeated daily, matter more than strict rules.
What meal or habit do you plan to try first this week? If helpful, keep exploring related posts for more practical meal ideas and symptom support.